Article by Baswati Sahoo* MS ,DNB,FRCS, FGAAS ,FRANZCO
Can someone have both cataracts and glaucoma?
Cataracts and Glaucoma often coexist in the elderly population and have a huge impact on their quality of life. Visual Impairment caused by cataracts or glaucoma has been associated with self-reported difficulties in physical function, emotional distress, and low socialization. While glaucoma causes irreversible peripheral vision loss, the central vision is often preserved until very advanced stages. A coexisting cataract affects this central vision. Cataract surgery enhances not just central vision but also clarifies the peripheral visual field for patients with glaucoma, ultimately improving their overall quality of life.
How do cataracts and glaucoma interact?
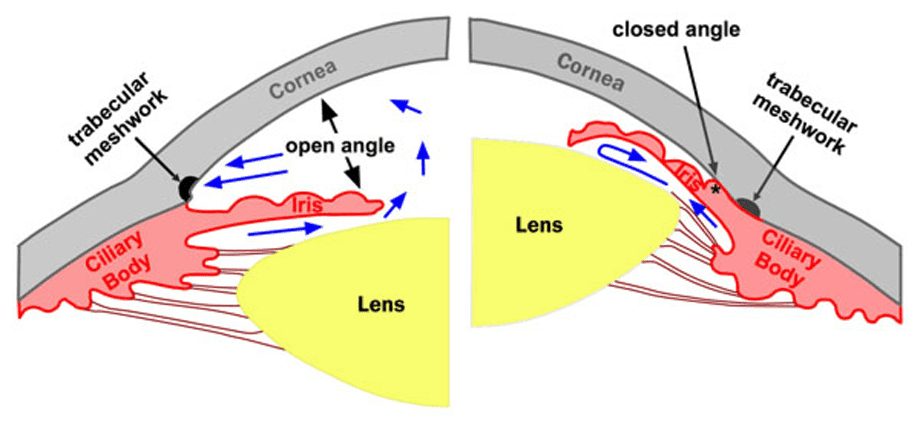
Glaucoma can be classified into open or closed angles based on the width of the anterior chamber angle in the eye. A cataract refers to the clouding of the eye’s natural lens. As it progresses, the cataract may begin to exert pressure on the iris, resulting in a narrowing of the anterior chamber angle, which could heighten the risk of angle-closure glaucoma, particularly in those who are already vulnerable to this issue. Essentially, the enlarged lens occupies more space in the eye, diminishing the area between the iris and cornea at the location where aqueous humor drains. This is important because aqueous humor must drain to maintain an optimum level of pressure within the eye. Pressure levels that are too high can cause irreversible glaucoma damage.
How can cataract surgery affect my glaucoma?
Cataract surgery entails replacing the clouded lens with a clear artificial one. Numerous studies show a moderate and lasting reduction in intraocular pressure (IOP) in patients with primary open-angle glaucoma and ocular hypertension after undergoing cataract surgery. IOP reductions tend to be more significant in patients with angle-closure glaucoma compared to those with open angles. One proposed explanation is that transitioning from a narrower angle with a naturally thicker lens (phakic angle), to a more open angle with an artificial, thinner lens (pseudophakic angle) enhances aqueous outflow.1 Another theory suggests that the tissue that drains fluid out of the eye (trabecular meshwork) expands.2 Johnstone et al. suggested that the aqueous outflow system functions like a mechanical pump. In glaucoma-affected eyes, this pump’s effectiveness diminishes due to the contact between the stiffening of the trabecular tissue and the walls of the channel (Schlemm’s canal) that collects and delivers aqueous humor into the bloodstream.3 Poley et al. suggested that cataract extraction improves this mechanical pump function.4
Is cataract surgery painful? Would I still need my glaucoma drops?
Phacoemulsification is the most common and advanced technique for cataract removal. This is a gentle eye surgery that eliminates cataracts and substitutes them with a synthetic lens. It can be conducted using topical or local anesthesia, ensuring that the procedure is both safe and pain-free. While cataract surgery can lead to a decrease in intraocular pressure, the necessity for glaucoma medication after the surgery is contingent upon the severity of glaucoma and the desired intraocular pressure for the eye. Additionally, minimally invasive glaucoma procedures, such as iStents and KDB glides, can be performed alongside cataract surgery, which may lessen the requirement for glaucoma drops.
Performing cataract surgery early in patients with glaucoma not only enhances their vision but also aids in more effective management of glaucoma. This approach should be recommended by all ophthalmologists.
References :
1.Shrivastava A, Singh K. The impact of cataract surgery on glaucoma care. Curr Opin Ophthalmol. 2014;25:19–25.
- Van Buskirk EM. Changes in the facility of aqueous outflow induced by lens depression and intraocular pressure in excised human eyes. Am J Ophthalmol. 1976;82:736–40.
- Johnstone MA. Pressure-dependent changes in configuration of the endothelial tubules of Schlemm’s canal. Am J Ophthalmol.1974;78:630–8. doi: 10.1016/s0002-9394(14)76301-9.
- Poley BJ, Lindstrom RL, Samuelson TW, et al. Intraocular pressure reduction after phacoemulsification with intraocular lensimplantation in glaucomatous and nonglaucomatous eyes: evaluation of a causal relationship between the natural lens and open-angle glaucoma. J Cataract Refract Surg. 2009;35:1946–55
*Clinical Lead and Consultant Ophthalmologist , Hawkes Bay Hospital
Refractive Cataract and glaucoma Surgeon , Eye Institute , Hawkes Bay