Detecting The Risk Factors
There’s no simple screening test for glaucoma. Glaucoma NZ recommends the “45 + 5 glaucoma eye examination”. People who have no symptoms of eye problems should have an examination for glaucoma by the time they are 45.
The emphasis is on detecting the risk factors for glaucoma and assessing the optic disc to decide the possibility of early glaucoma being present. If the examination is normal we recommend it be repeated every 5 years. Those with risk factors for glaucoma (such as a family history of glaucoma or steroid use) should be examined earlier, and more frequently.
So what should you expect at a routine glaucoma eye examination?
Three essential elements of a glaucoma eye examination are:
- Measuring eye pressure
- Examining the optic disc
- Visual fields testing
However, there are several other kinds of investigations that you may experience, including photography, gonioscopy (when the angle of your eye is measured), scanning of the optic disc and nerve fibre layer, and measuring of central corneal thickness.
Risk Factors10 Facts About Glaucoma
Prof Helen Danesh Meyer, Glaucoma Neuro-Ophthalmology & Cataract Surgeon presents the 10 Basic facts about Glaucoma that everyone should know. This talk was presented at the GNZ Glaucoma Patient Symposium 2020.
How often should you have an eye exam?
We recommend everybody 50 years or older visit an optometrist every 2 years for a comprehensive eye exam, and if you have a family history of glaucoma or are of Asian or African descent we recommend you get your eyes checked every 2 years from the age of 40.
If you have a family member that has advanced glaucoma, it is recommended that you commence having regular eye health checks earlier.
As well as checking whether you need glasses, an optometrist will carry out different tests to check the health of your eye. These tests are key to detecting glaucoma.
What to expect when you have your eye exam
It is important to remember that glaucoma cannot be self-detected. Only an ophthalmologist or optometrist can determine whether you have glaucoma.
During a glaucoma exam your eye health practitioner will:
- Measure your intraocular pressure (IOP) also called your eye pressure.
- Examine your eye’s drainage angle.
- Check your optic nerve for damage.
- Test your central and peripheral (side) vision.
- Take images or computer measurements of your optic nerve.
- Measure the thickness of your cornea.
Glaucoma NZ has put together a useful checklist to take with you to your eye exam.
Tests for Glaucoma
Visual Field Testing (Perimetry)
How much we can see of the world around us is known as our visual field. Glaucoma first damages our visual field.
If you hold your vision on one spot you will be aware that everything in the centre is clear, but becomes less and less clear the further away from the centre an object is.
When we close one eye we see the world through an oval shaped hole which is referred to as our peripheral visual field. Because we have two eyes and a large percentage of our visual field is contributed to by both eyes seeing the same thing, it is possible to lose quite significant portions of our visual field and yet be unaware of it.
Visual field tests are designed to map a person’s visual field; to document the extent of peripheral vision. As most glaucoma patients know, the test consists of responding every time a flash of light is perceived while looking straight ahead.
If doctors relied only on a reduced visual field to detect glaucoma, they would miss most people with early glaucoma. That is why field-testing is only one part of a glaucoma evaluation. If doctors suspect a person may have glaucoma a visual field test may help confirm or rule out glaucoma. The visual field also provides essential information about whether the glaucoma is stable or is getting worse.
The perimetry test takes around 3-6 minutes per eye and is repeated 1-2 times a year so that every new test can be compared to the previous ones to look for any worsening.
Eye Pressure Test (Tonometry)
Tonometry measures the pressure within the eye. One of the main risk factors for glaucoma is high eye pressure and lowering the eye pressure is the best treatment for glaucoma. Accurate measurement of the eye pressure (tonometry) is essential for glaucoma treatment. The Goldman Applanation Tonometer is the most accurate way of measuring the eye pressure. It involves numbing the eye with eye drops first and then the instrument gently contacts the front of the eye to take the measurement.

Accurate measurement of eye pressure assesses this important risk factor and shows how effectively your glaucoma medications are working. For best comparison of measurements, the time of day and the time from the last use of glaucoma medications should be recorded. Frequent measures of eye pressure would detect peak levels and fluctuation.
What eye pressure doesn’t tell you is whether the glaucoma damage to your optic nerve is stable or progressive. That can only be determined by assessing the optic nerve head or testing the visual field.
The perimetry test takes around 3-6 minutes per eye and is repeated 1-2 times a year so that every new test can be compared to the previous ones to look for any worsening.
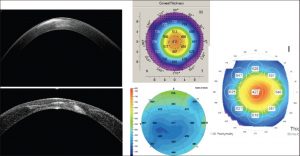
OCT (Optical Coherence Tomography)
An OCT scan is an important test in diagnosing and monitoring glaucoma. It is used to measure the retinal nerve fibre layers (RNFL) around the optic nerve which is an important marker of early to moderate glaucoma damage. For glaucoma suspects and those at the very early stages of glaucoma, the visual field test may not show any peripheral field damage however, the measurements from the OCT can detect early signs of glaucoma.

The OCT measurements can also help monitor any changes and progression with glaucoma. This can help determine the treatment plan.
Drainage Angle Outflow (Gonioscopy)
Gonioscopy is the examination of the drainage angle for the outflow of intraocular fluid. Fluid is constantly being made in the eye and it flows out of the eye at the drainage angle. This test can determine if the high eye pressure is caused by a closed/blocked angle (angle closure glaucoma) or if the angle is open but just not working well enough (open angle glaucoma). This is important because the management of each sub-type is slightly different. The test involves putting a mirrored lens on the surface of the eye after using a numbing drop, almost like wearing a contact lens.

Optic Nerve Check (Ophthalmoscopy)
Ophthalmoscopy is the visual examination of the optic nerve. Since glaucoma is a disease of the optic nerve, this is a key test. Dilating drops are usually given to enlarge the pupil, so that the optic nerve can be more clearly seen. The nerve(s) will be looked at for signs of glaucoma-related nerve cell loss. This can be done using a table top slit lamp or hand held ophthalmoscope. The appearance of the optic nerve can be documented with a drawing, a photo or with an imaging device. This is so any worsening of the nerve appearance can be detected in the future.
Corneal Thickness (Pachymetry)
Pachymetry is a test that measures the thickness of the front window of the eye (cornea). The eye is numbed with drops then a contact probe quickly measures the thickness in a few seconds. A very thick or very thin cornea can affect the pressure/tonometry readings and also a very thin cornea increases the risk of developing glaucoma.